Understanding

Understanding
Retroperitoneal
Fibrosis (RPF):
Key Facts to know
What is the Retroperitoneum
What is the Retroperitoneum
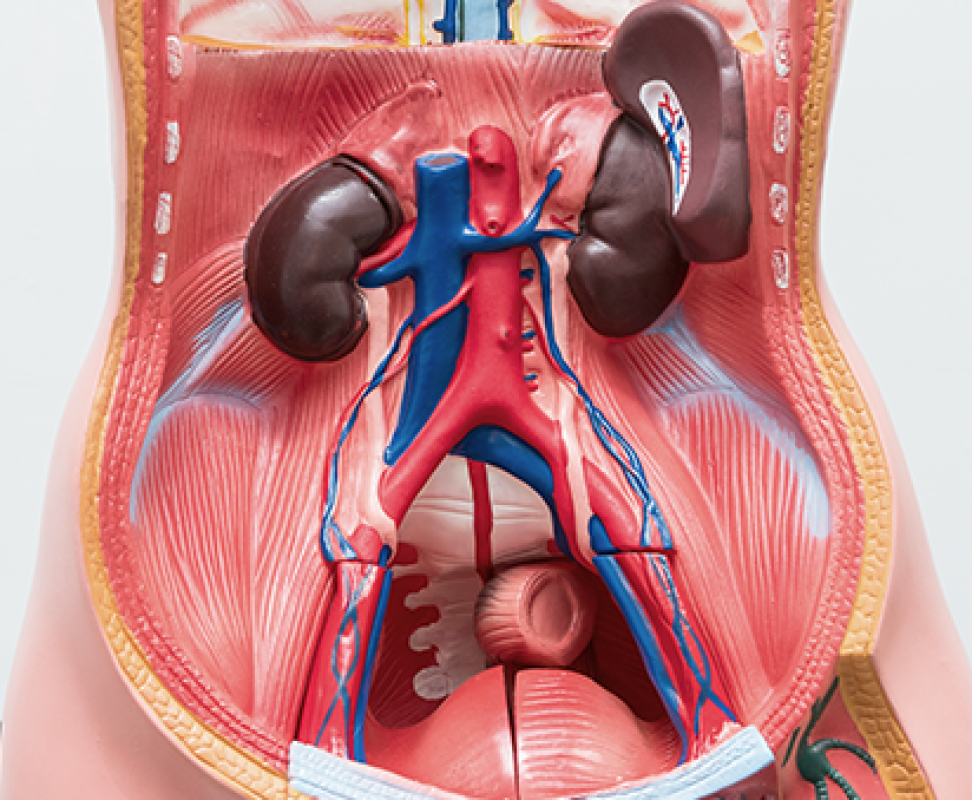
The abdominal cavity is separated into two main compartments by a membrane called the PERITONEUM. The PERITONEUM is a smooth membrane that lines the abdominal cavity and covers many of the abdominal organs. The peritoneum is made up of two layers. One layer – the PARIETAL PERITONEUM – is the layer that lines the abdominal cavity and the walls of the pelvis. The other layer is the VISCERAL PERITONEUM, which is the layer that is on the abdominal organs. The space between the parietal and visceral peritoneum is called the PERITONEAL CAVITY.
The organs that are located between these two layers are considered INTRA-PERITONEAL and include things like the stomach, liver, spleen, most of the small bowel (i.e. 1st part of the duodenum, jejunum, and ileum) and certain parts of the large bowel (i.e transverse colon, sigmoid colon).
The area of the abdomen and the pelvis (posterior) to the peritoneum is called the RETROPERITONEUM.
The organs in the RETROPERITONEUM include:
• Kidneys
• Adrenal glands (tissue on top of the kidneys that make regulatory hormones)
• Pancreas
• Part of the small bowel (2nd/3rd part of the duodenum)
• Part of the large bowel (ascending and descending colon)
• Major blood vessels
• Aorta
• Inferior vena cava (the large vein that runs alongside the aorta)
What is RPF
What is RPF
RETROPERITONEAL FIBROSIS (RPF) is term used when there is evidence of excessive inflammatory and fibrous (‘scar’) tissue in the retroperitoneal space. This collection of fibrous tissue can result in development of a soft tissue mass. Depending on the location of the mass, certain things can be impacted in the retroperitoneum.
When the soft tissue thickening is centered around the aorta it is most commonly referred to as ‘CHRONIC PERIAORTITIS’ (CP).
The most common location of RPF/CP is around the aorta below the kidney (renal) arteries. This part of the aorta is called the INFRARENAL ABDOMINAL AORTA. It most often surrounds the anterior and lateral sides of the aorta and extends from the level of the kidney (renal) arteries down to where the aorta splits into the common iliac arteries.
Types of RPF
Types of RPF
There is no standardized agreement on the naming of terms related to retroperitoneal fibrosis. Some providers and researchers separated retroperitoneal fibrosis into two main groups; PRIMARY (Idiopathic) and SECONDARY
Primary
PRIMARY is thought to be due to a malfunction, or over-activity, of the immune system (immune-mediated) and accounts for 60-70% of RPF cases.
The PRIMARY category is further divided into:
• Idiopathic – meaning the cause is unknown
• IgG4 related disease (IgG4-RD) – a condition characterized by certain tissue (lymphocytes and plasma cells) that infiltrate into tissue associated with secretion of a protein (antibody) called Immunoglobulin G subclass 4.
Secondary
Secondary retroperitoneal fibrosis is where there is another cause or disease that has led to the development of the inflammatory/fibrotic mass.
These include:
Drugs: some medications have been associated with an increased risk of RPF including certain headache medications like methysergide and ergotamine. Some immunosuppressive medications like tumor necrosis factor inhibitors (e.g. etanercept/Enbrel and infliximab/Remicade) have also been associated with causing RPF, but the mechanism of why this occurs is unknown
Cancer: Some cancers like Carcionoid tumors and Lymphoma have been associated with retroperitoneal fibrosis / periaortitis. Metastatic disease from breast, prostate, bladder, pancreas, or colorectal cancer can results in RPF.
Infections: Certain infections like tuberculosis, histoplasmosis, and other atypical infections can results in retroperitoneal fibrotic soft tisssue collections.
Radiation: Treatment with radiation therapy to the abdomen or pelvis for cancer can result in fibrosis in the retroperitoneum. This can develop even years after the radiation.
Surgery: Surgery or complications from surgery (like bleeding or infection) can result in development of retroperitoneal fibrotic tissue.
Histiocytic disorders: Conditions like Erdheim-Chester Disease (ECD) and Rosai Dorfman Disease (RDD) are conditions that are technically cancers but the infitrate is a certain type of white blood cells called macrophages/histiocytes.
Symptoms of RPF
Symptoms of RPF
The symptoms of retroperitoneal fibrosis can be non-specific and therefore it can be hard to tell that something is going on.
The most common symptoms of RPF are:
• Back pain
• Flank (sides of back / under rib) pain
• Lower abdomen / pelvic pain
• Change in urination (reduction)
• Leg swelling (one side or both)
If the urine is not able to get out adequately then the kidney function may decline, in some circumstances rapidly.
Complications of RPF
Complications of RPF
While pain is important to control, the most important things to manage are the kidneys and the veins.
Kidneys
The soft tissue mass can result in narrowing or obstruction of the URETERS. The ureters are the tubes from the kidney to the bladder. If the ureters are obstructed then the urine cannot get out and it backs up into the kidney (a finding called HYDRONEPHROSIS). When this occurs the kidney function declines. If this occurs for too long before being recognized it can result in ACUTE KIDNEY FAILURE or CHRONIC KIDNEY DISEASE.
The most important immediate management is alleviating the obstruction through use of ureteral STENTS or tubes inserted from the outside into the kidney (NEPHROSTOMY TUBES).
Veins:
The soft tissue mass can compress the veins in the abdomen (e.g. inferior vena cava) or pelvis (iliac veins). When the veins are compressed, blood is not able to return from the legs back up to the heart and as a result the legs can swell. Often providers will check the lower legs to check for blood clots (called deep vein thrombosis or DVT) but the ultrasound of the legs are ‘negative’ for blood clot because the clot is higher up in the pelvis and not seen with ultrasound of the legs. In those cases, an evaluation with ultrasound OR CT scan of the pelvis veins is needed to confirm where the narrowing occurs.
How to Evaluate RPF
How to Evaluate RPF
Retroperitoneal fibrosis is identified on imaging studies such as a computed tomography (CT) scan, magnetic resonance imaging (MRI) scan, or Positron-Emission Tomography (PET) scan.
The classical location of soft tissue mass for retroperitoneal fibrosis is around the aorta, below the kidney (renal) arteries with termination at the level of the iliac arteries.
Biopsy should be considered to assist in diagnosis – especially if there are atypical features of the soft tissue.
Atypical features include:
•Large lymph nodes (lymphadenopathy)
•‘Infiltrative’ tissue into the muscle, bone, or other structures
•Abnormal location of tissue:
Pelvic wall
Peri-ureteral (around the ureter)
Peri-bladder (around the bladder)
Peri-pancreatic (around/near the pancreas)
Peri-duodenum (around/near the small intestine)
Peri-colonic (around/near the colon)
Peri-renal (around the kidney)
How is a biopsy obtained:
CT guided: This is where a needle is placed from the outside under guidance with a CT scan. This is typically done by an INTERVENTIONAL RADIOLOGIST. This is the most common type of biopsy performed for retroperitoneal fibrosis.
Laparoscopic: Also called, minimally invasive surgery - this is where small incisions are made (typically two or three) and a small flexible tube with a camera is inserted with another instrument to take the tissue sample. This is typically done by a GENERAL SURGEON.
Laparotomy: Also called, open surgery – this is where a surgeon makes an incision (cut) into the abdomen to gain access to the abdomen/pelvis where a biopsy of the soft tissue can be made.
What other testing should be done?
Laboratory testing should include:
• Complete Blood Count (CBC) with differential
• Kidney function (Creatinine)
• Urinalysis with microscopy (urine study)
• IgG4 level (blood)
• Inflammatory markers (ESR, C-reactive protein)
• Additional optional labs might include:
• Liver function testing
• Tuberculosis testing
• Histoplasma antibodies
• Autoimmune labs
• Imaging: Depending on suspicion of IgG4-RD or Secondary causes, additional imaging may be needed including – CT (or MRI) of the chest or PET-CT scan.
These studies can determine if there are any other soft tissue collections / masses elsewhere in the body.